Pregabalin to buy uk Can Testosterone Replacement Therapy Hurt and Lower Sperm Counts after Vasectomy Reversals? 2023 Update
buy provigil modafinil Yes, it is well known that men who are taking testosterone replacement therapy usually have significant suppression of sperm production. Sometimes this can be total suppression so that the testicles do not make any sperm at all, called azoospermia. Other times, sperm production is just dramatically lower than normal. Sperm production usually comes back over time after the testosterone replacement is stopped and as the body gradually resumes normal testicular function, but not always.
This article, compiled by global vas reversal authority, surgeon and author Dr. Sheldon Marks, discusses the concerns about men on testosterone replacement therapy and the unintended negative impact on sperm production and fertility after a vasectomy reversal.
How quickly sperm counts return to normal levels depends on multiple factors, including
1. the dose of the testosterone taken every week or two and
2. how long each person was on the hormone replacement therapy. In general, the higher the dose and longer the person was on testosterone, the longer it will take for sperm production to bounce back. There are some men who don’t have much suppression, others who stay suppressed to varying degrees and some who never have a return to their normal sperm count levels (1).
There is no way to accurately predict which men will have which response.
How does testosterone replacement therapy drop sperm production?
Testosterone replacement suppresses sperm production because the brain functions as a thermostat to set each person’s optimal, DNA driven testosterone level. When the brain senses elevated testosterone levels as a result of the added replacement testosterone higher than it wants, the brain shuts down the natural hormone production. The issue is that LH, the hormone that stimulates testosterone secretion that is shut down with testosterone replacement is directly linked to FSH, the hormone that stimulates sperm production. This means that for most men, when LH is suppressed because of the high testosterone levels, so the FSH is also blocked, which is why sperm counts become suppressed or are zero as well.
 Why is this important with a vasectomy reversal?
Why is this important with a vasectomy reversal?
Why is it ideal to have sperm production back to normal levels at time of the vas reversal?
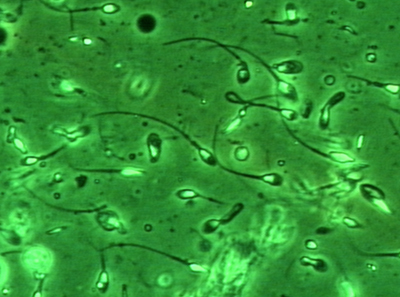
During the reverse vasectomy surgery after the vasectomy scar is removed, the fluid that comes out of the vas is analyzed under the lab microscope to look for the presence or absence of sperm to tell the urologist whether the system is open or blocked. If sperm are seen in the vasal fluid, then that confirms the system is open and sperm are getting through so it is correct for the doctor to perform a vas-to-vas connection. If no sperm are seen, often in thick, pasty vasal fluid, then this confirms that there is deeper blockage down in the epididymis and so a vas-to-epididymal connection is the correct technique needed to bypass the blockage (2). Performing the vas-to-vas connection when no sperm are seen usually means that connection on that side will not usually be successful.
What if a man is on testosterone and no sperm are seen in the vasal fluid during the vas reversal?
In this situation, the dilemma is that the urologist won’t know whether the absence of sperm in the fluid from the vas is because the testosterone is suppressing sperm production (and so a vas-to-vas is the correct connection) or because of deeper epididymal blockage, and so the vas to epididymal connection is indicated). When a man is taking testosterone, the doctor may not know which is the correct technique, vas-to-vas or vas-to-epididymal bypass, to perform. If sperm production is back to normal, then we should see sperm and we will not be confused by a lack of sperm in the fluid.
Is there any other way to know if there is normal sperm production if no sperm are seen in the fluid from the vas?
Yes, at our center, because we have a full-time senior andrologist, the surgeon can perform a microbiopsy of the testicle through a tiny needle hole and then and hand off the specimen to the andrologist who can analyze that tiny speck of tissue and see if normal sperm production (spermatogenesis) is present. If no sperm are seen, then we know that sperm production is suppressed from the testosterone therapy.
What if my doctor didn’t warn me or explain that taking testosterone can hurt sperm production ?
Sadly, many doctors and even some urologists don’t know or understand the mechanisms of how a man taking testosterone therapy can hurt sperm production. Many doctors are being taught that if a man has low testosterone levels then he should get testosterone replacement rather than looking for the cause of the low testosterone or asking about future fertility wishes. I have even had a few doctors argue with me and tell me that the concerns about sperm suppression with testosterone replacement therapy wasn’t true and I was just “making this all up” (3).
What should be done if a man is still on or was recently taking testosterone before the vasectomy reversal?
If a man is considering a vasectomy reversal for restoration of fertility, it is best if he contacts his doctor ASAP to get guidance to work with his local doctors to stop the testosterone replacement immediately. In our practice, we also ask to send us all previous lab test results. If there are not any hormones level results tested recently, then it would be a good idea to go ahead and check a hormone panel including a testosterone, FSH, LH and estradiol levels (to be drawn between 8 and 10 AM) and have these results sent to us as well. We are always happy to talk with or email with patient’s own personal doctors explaining what we would do and to answer any questions about restoring the man’s sperm production and naturally boost his testosterone levels.
How should sperm production be restored after stopping testosterone therapy?
Many men with suppressed sperm production can have their fertility restored and even accelerated by stopping the testosterone immediately and taking certain prescription medications (clomiphene citrate, also called Clomid pills, and/or HCG injections). While we often can’t prescribe these before the vas reversal, we frequently work with each person’s local doctors to get hormone levels and testosterone back up to normal. What is nice is that these medications also stimulate the body’s own natural testosterone production as well as sperm production, so men don’t feel any long-term symptoms of stopping the testosterone. Some men do not want to wait and so we can go ahead and perform the vasectomy reversal and during the surgery use the doctors’ judgment and discussion with the patient, based on multiple factors, to decide if a Vas-to-Vas or Vas-to-Epididymis connection is indicted.
Call us anytime to answer any questions at (888) 722-2929 for more information about testosterone, fertility or vasectomy reversal success rates and when ready, to set up a no-cost consult with either Dr. Marks or Dr. Burrows at our full-time, vas reversal only “center of excellence” here in Tucson, Arizona, where every day we see men from every state in the US and more than 85 countries around the world.
This page was reviewed, edited and updated January 1, 2023, by Sheldon H. F. Marks, MD.
References:
1. Coward RM, Mata DA, Smith RP, Kovac JR, Lipshultz LI. Vasectomy reversal outcomes in men previously on testosterone supplementation therapy. Urology. 2014 Dec;84(6):1335-40.
2. Kirby EW, Hockenberry M, Lipshultz LI. Vasectomy reversal: decision making and technical innovations. Transl Androl Urol. 2017 Aug; 6(4): 753–760.
3. Kovac JR, Scovell J, Ramasamy R, Rajanahally S, Coward RM, Smith RP, Lipshultz LI. Men regret anabolic steroid use due to lack of comprehension regarding the consequences on future fertility. Andrologia, 2015 Oct;47(8):872-8).