Why Is a Semen Analysis Important after Vasectomy Reversal
Following a vasectomy reversal, a series of semen analysis tests are very important to monitor progress of the healing and to ensure a full return of fertility. ICVR recommends the first post-operative semen analysis at http://offsecnewbie.com/wp-json/wp/v2/posts/1160 4 weeks following the vasectomy reversal, and then every 4 weeks as directed (1).
This educational article, by our andrologist Matthew F. Marks, MS, TS (ABB), of Arizona Andrology Lab and Cryobank, explains some key concepts about understanding the meaning of key numbers of a semen analysis after vasectomy reversal.
It is important to remember that a semen analysis is obligingly not a measure of fertility but instead is only a measure of sperm production AND sperm delivery.
Having this information is key to achieving the highest results from the vasectomy reversal aftercare. Low or dropping sperm counts or motility can be a sign of inflammation or scarring at the connection site and the need for anti-inflammatory medications (2).
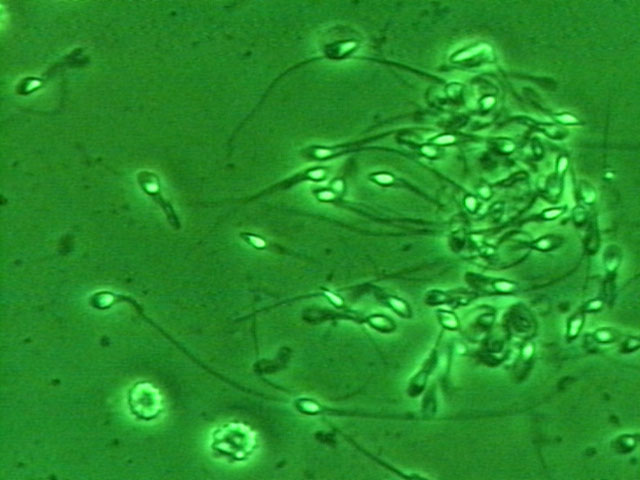 When interpreting the semen analysis results after the vas reversal, it is important to focus on three main numbers; the fluid volume (cc or ml) of that specimen, the sperm concentration (or count, how many million sperm per ml or cc), and the % motility.
When interpreting the semen analysis results after the vas reversal, it is important to focus on three main numbers; the fluid volume (cc or ml) of that specimen, the sperm concentration (or count, how many million sperm per ml or cc), and the % motility.
A sperm count is nothing more than a single snapshot of a constantly fluctuating output of sperm. It is like looking at a single frame of a movie and trying to guess all the details of the plot and characters. Yes, many can get some information from a single semen analysis but it is not wise to over-interpret and make assumptions about the findings from just one count. It is important to understand that the semen analysis results will normally fluctuate from test to test, over time as well as lab to lab. So when looking at numbers, think in terms of “ballpark” results. For example, if the concentration goes from 43 million to 39 million, that is likely just from expected normal fluctuations. Likewise, a change in motility from 38% to 31% is also probably not anything of concern.
As we check these numbers over time, if there is a real trend with the numbers dropping, then that is more likely real and would need treatment. We also would review many issues with lifestyle, medications and work to be sure that nothing is being done that can drop sperm counts.
 When we look at sperm counts, we look at the individual numbers of these three parameters and then multiple them together to calculate the total motile count, which is the total number of motile sperm in that single specimen (TM). This is really the only number that is truly important after a vasectomy reversal! Sometimes one number will go up and another will go down but the total motile will be about the same.
When we look at sperm counts, we look at the individual numbers of these three parameters and then multiple them together to calculate the total motile count, which is the total number of motile sperm in that single specimen (TM). This is really the only number that is truly important after a vasectomy reversal! Sometimes one number will go up and another will go down but the total motile will be about the same.
Ideally the volume should be about 1.5 ml or higher, the concentration 20 million/ml or higher, and motility 50% or higher which comes out to a total motile count of 15 million motile sperm or higher (3). If a man has at least 10 to 15 million motile sperm in the sample then he should have no problems conceiving, assuming there are no underlying female factors. Interestingly, there are many couples that have no trouble conceiving naturally with surprisingly low numbers and other couples may have delays or issues even with high normal sperm parameters.
Oftentimes after a reversal the numbers start off lower and then go up over time, so do not be upset if the counts or motility are low in the early phases (4). Again, the trends over time are what is important.
If anyone has specific questions before or following a vasectomy reversal, both Dr. Sheldon Marks or Dr. Peter Burrows are available to talk at (888) 722-2929 .
References:
1. Marks SHF. Vasectomy Reversal: Vasovasostomy and Vasoepididymostomy. New York; Springer; 2018.
2.Perkins A, Marks MB, Burrows PJ, Marks SF. Anti-Inflammatory Treatment for Asthenozoospermia Following Microsurgical Vasectomy Reversal. Presented at American Society of Andrology 38th Annual Meeting, San Antonio, Texas: April 13-17, 2013.
3.World Health Organization. WHO laboratory manual for the examination and processing of human semen. 5th ed. 2010.
4.Perkins A, Marks M, Burrows P, Marks S. Sperm kinetics following vasectomy reversal. Androl 2012;33(Suppl2):42).
This page was reviewed, edited and updated August 13, 2022 by Sheldon H. F. Marks, MD.