How Should the Vasectomy Reversal Surgeon Choose a VV or VE in 2023?
This article, by vasectomy reversal authority, author and microsurgeon Sheldon Marks MD, updated in 2023, reviews how doctor’s decide whether to perform a vas-to-vas (VV, vasovasostomy) or vas-to-epididymal bypass (VE, vasoepididymostomy) during the surgery and why this is so critically important to achieve the highest vas reversal success rates.
Deciding which technique to perform that is best for that side and for that patient is considered the most critical decision each surgeon must make during the surgery. When done correctly, this thought process will ensure the very highest chances for success of a reverse vasectomy. Sadly, this straightforward decision-making that is taught at every course, in every class and in the textbook on reversals is the one most commonly ignored by many doctors throughout the US and around the world.
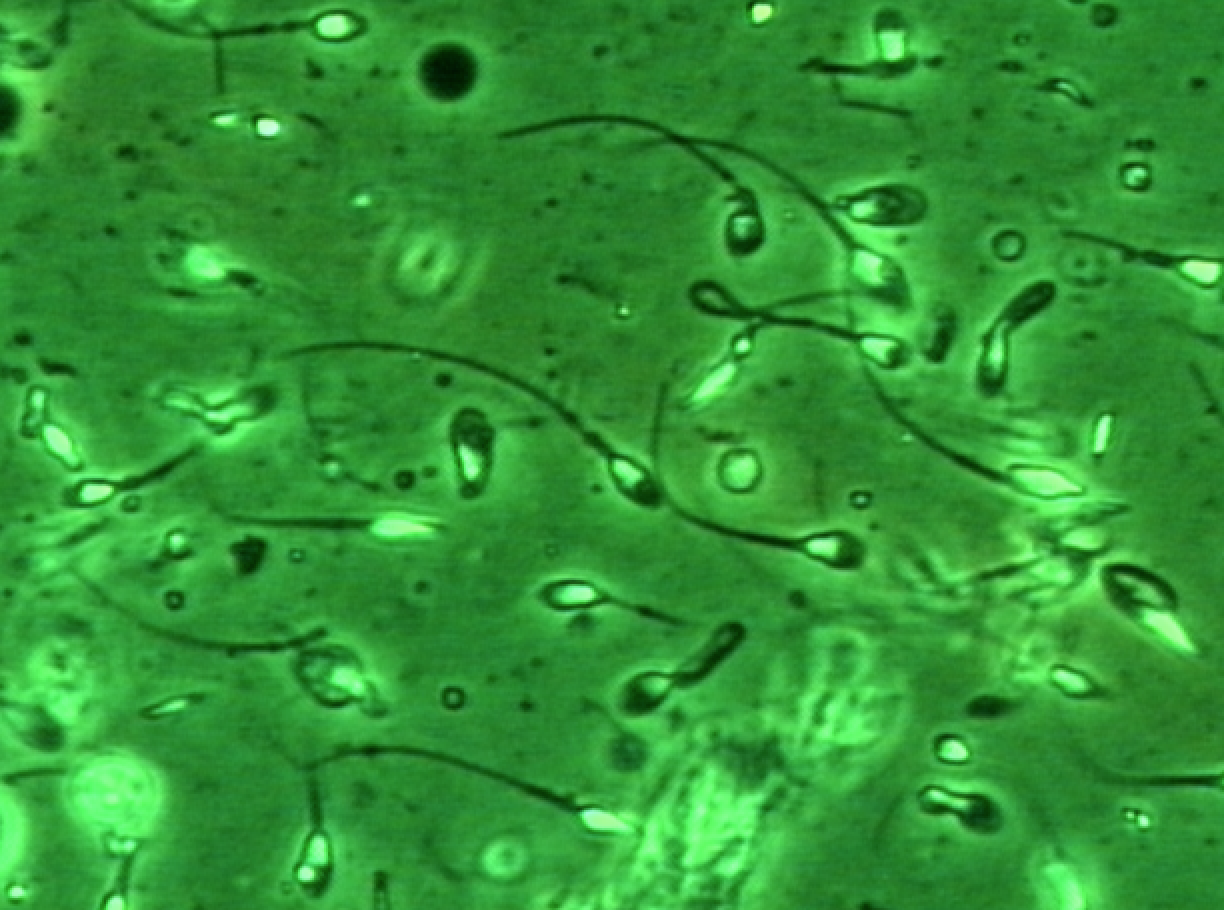 http://solent-art.co.uk/tag/watercolour/ Open or blocked? The big question during the reverse vasectomy is whether or not the tubes within the testicle, epididymis and vas are all open and sperm are passing through into the vas or if there is deeper epididymal blockage preventing the sperm from getting to the vas. During the vas reversal, after we cut across the vas just below the vasectomy scar, our andrologist analyzes a tiny drop of fluid from the vas under a high power lab microscope. If sperm or sperm parts are seen microscopically in the vasal fluid, then we know that the “system” is open all the way from the testicle through the epididymis to the vas and so a straightforward vas-to-vas (VV) connection is the http://preferredmode.com/tag/pink/ correct connection to be performed (1).
http://solent-art.co.uk/tag/watercolour/ Open or blocked? The big question during the reverse vasectomy is whether or not the tubes within the testicle, epididymis and vas are all open and sperm are passing through into the vas or if there is deeper epididymal blockage preventing the sperm from getting to the vas. During the vas reversal, after we cut across the vas just below the vasectomy scar, our andrologist analyzes a tiny drop of fluid from the vas under a high power lab microscope. If sperm or sperm parts are seen microscopically in the vasal fluid, then we know that the “system” is open all the way from the testicle through the epididymis to the vas and so a straightforward vas-to-vas (VV) connection is the http://preferredmode.com/tag/pink/ correct connection to be performed (1).
What if no sperm are seen? If the fluid from the vas looks thick or toothpaste-like, and there are no sperm or sperm parts seen microscopically, then this tells us that most often there is a deeper obstruction in the epididymis which blocks the flow of sperm from the testicle out to the vas. When we see this, we know that a vas-to-vas connection has an extremely low chance for success, if at all. When there are no sperm seen, leading vas reversal experts agree that the correct vasectomy reversal procedure is to perform the more challenging vas-to-epididymal connection (VE) to bypass the blockage and restore the flow of sperm out to the vas (2).
Dr. Marks recently posted an educational video on the SSMR (Society for the Study of Male Reproduction) YouTube channel, designed to help other vas reversal doctors to understand this decision-making process with all of the primary as well as additional factors that contribute into which connection is performed.
This video can be viewed at https://www.youtube.com/watch?v=oe27StapecI.
The right way. When we work with other top experts to teach classes to other urologists on how to perform vas reversals or we write textbooks or chapters and andrology certification courses, it is very clear that true experts explain how this decision-making process is in the patient’s best interest for doctors when they perform vasectomy reversals. It is made very understandable that to practice within the appropriate “standard of care,” all doctors who perform vas reversals should:
1. Always microscopically analyze the fluid from the vas and
2. Have the training, skill and expertise and be willing and able to perform the epididymal bypass (VE) when needed (3).
Number of years. Knowing that men as soon as 2 to 3 years from vasectomy may need an epididymal bypass, and up to 1/3 of men will need a bypass on at least one side at 8 to 10 years out from vasectomy, vasectomy reversals thought leaders believe that all doctors that perform vas reversals should be willing and able to perform the bypass when indicated and not limit their practice to a “one size fits all” and only perform a vas-to-vas connection on all patients (4).
Here at ICVR, America’s premier full time, vas reversal only center, we have a proven, published success rate of up to 99.5% (5) for a vas-to-vas connection and a 70 to 90% success for a vas-to-epididymal bypass. Another smart reason to consider ICVR for a vasectomy reversal.
Call our office to have any questions answered, (888) 722-2929 .
And when ready, our senior staff of reverse vasectomy professionals can also set up a no-charge consultation with one of our two doctors, Dr. Sheldon Marks or Dr. Peter Burrows, by phone, Zoom, Skype, Face Time or in office.
This page was reviewed, edited and updated January 1, 2023, by Sheldon H. F. Marks, MD.
References:
1. Mui P, Perkins A, Burrows PJ, Marks SF, Turek PJ. The need for epididymostomy at vasectomy reversal plateaus in older vasectomies: a study of 1229 cases. Androl 2014;2(1):25-9.
2. Kirby EW, Hockenberry M, Lipshultz LI. Vasectomy reversal: decision making and technical innovations. Transl Androl Urol. 2017 Aug; 6(4): 753–760.
3. Chawla A, O’Brien J, Lisi M, Zini A, Jarvi K. Should all urologist performing vasectomy reversal be able to perform vasoepididymostomies if required? J Urol 2004;172(3):1048-50.
4.Marks SHF, Burrows PJ, Cropp AR, Ax RL, McCauley TC. Obstructive interval should not be a deterrent in vasectomy reversal. Androl 2008;March/April(Suppl):21.
5.Crosnoe LE, Kim ED, Perkins AR, Marks MB, Burrows PJ, Marks SH. Angled vas cutter for vasovasostomy: technique and results. Fertility and Sterility.2014;101(3):636-639.